What Every Man Should Know About hCG
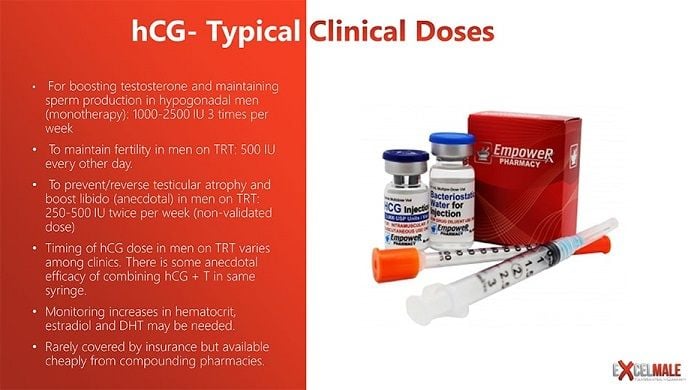
Table of Contents
What is Human Chorionic Gonadotropin (hCG) and How it Can Help Men?
- HCG (human chorionic gonadotropin) is produced by the human placenta, a sterile product derived from the urine of pregnant females. Recombinant DNA formulas are produced by pharmaceutical companies and compounding pharmacies.
- In men, HCG mimics LH from the pituitary to stimulate Leydig cells of testes to produce testosterone.
- It can have an additive effect on testosterone replacement therapy's ( TRT) increases in estradiol, hematocrit and/or acne
- The normal lyophilized vial contains 5,000 or 11,000 units HCG by compounding pharmacies (commercial products cost 3X compounding). The vial is sent with bacteriostatic water for reconstitution.
- Used by fertility specialists to induce ovulation to harvest eggs, and sperm production.
- The latest data show that men on TRT + HCG were able to remain fertile. (TRT + 500 IU HCG every other day)
- The usual dose of 350-500 IU two times a week for the prevention/reversal of testicular atrophy. No data have been published on this use.
- Anecdotal effect on raising sex drive in men. No data.
- HCG acts as a Leydig cell stimulator and cell volumizer. Testicles regain size but do not grow beyond baseline size.
- Continuous testosterone can reduce fertility in over 50% of TRT users and testicular size by 10-30 %. HCG may reverse those two issues.
- Noticeable testicular size reduction can be a more common complaint in men with smaller testicular size at baseline. It may not be important to some older men or men not worried about fertility.
- HCG may be used in patients who have abused steroids for 6-8 weeks before c l omiphene to attempt to accelerate the natural production of testosterone.
- May be used in younger males as the sole method of testosterone treatment with secondary hypogonadism. All men respond differently to HCG's ability to boost T production by testes. Expensive as monotherapy and frequently used with testosterone replacement since that combination may be more cost-effective in normalizing testosterone and fertility.
- HCG may reactivate upstream hormones like pregnenolone and progesterone that are shut down by testosterone replacement therapy.
- HCG may not work well in some men who have primary hypogonadism, i.e. dysfunction of the Leydig cells in the testes.
How Does hCG Work in Men?
HCG + TRT Studies
HCG mimics LH but it is not LH and it's not picked up by the LH blood test. In fact, it suppresses LH as endogenous testosterone does. But the amazing thing that the first study below found is that HCG can increase sperm production and quality even in the absence of LH and FSH. Most researchers believed that without FSH there was no possible sperm production.
The second study shows that testosterone inside the testicles (intratesticular testosterone or ITT) has to reach a certain amount for Sertoli cells to "wake up" to produce sperm. TRT actually decreases testosterone inside the cells by an unknown mechanism. HCG doses under 300 IU along with TRT may not normalize intratesticular testosterone since 250 IU produced an ITT 7% below baseline. 500 IU produced ITT 25% above normal. The Baylor study below used the 500 IU dose.
Testosterone+ HCG Preserves Healthy Sperm in Men on Testosterone Replacement Therapy (Injections and gels)
Tung-Chin Hsieh, Alexander W. Pastuszak, Kathleen Hwang and Larry I. Lipshultz
From the Division of Urology, University of California-San Diego (TCH), San Diego, California, Scott Department of Urology, Baylor College of Medicine (AWP, LIL), Houston, Texas, and Department of Urology (KH), Brown University School of Medicine, Providence, Rhode Island
Purpose: Testosterone replacement therapy results in decreased serum gonadotropins (hormones produced by the pituitary gland- LH and FSH- that jump-start testicular function) and intratesticular testosterone (inside the testicles), and impairs spermatogenesis (sperm production), leading to azoospermia (no viable sperm) in 40% of patients. However, intratesticular testosterone can be maintained during testosterone replacement therapy with co-administration of low dose human chorionic gonadotropin, which may support continued spermatogenesis in patients on testosterone replacement therapy.
Materials and Methods: We retrospectively reviewed the records of hypogonadal men treated with testosterone replacement therapy and concomitant low dose human chorionic gonadotropin(HCG). Testosterone replacement consisted of daily topical gel or weekly intramuscular injection with intramuscular human chorionic gonadotropin (500 IU) every other day. Serum and free testosterone, estradiol, semen parameters, and pregnancy rates were evaluated before and during therapy.
Results: A total of 26 men with a mean age of 35.9 years were included in the study. The mean follow-up was 6.2 months. Of the men, 19 were treated with injectable testosterone and 7 were treated with transdermal gel. Mean serum hormone levels before vs during treatment were testosterone 207.2 vs 1,055.5 ng/dl (p<0.0001), free testosterone 8.1 vs 20.4 pg/ml (p = 0.02) and estradiol 2.2 vs 3.7 pg/ml (p = 0.11). Pretreatment semen parameters were volume 2.9 ml, density 35.2 million per ml, motility 49.0% and forward progression 2.3. No differences in semen parameters were observed during greater than 1 year of followup. No impact on semen parameters was observed as a function of testosterone formulation. No patient became azoospermic during concomitant testosterone replacement and human chorionic gonadotropin therapy. Nine of 26 men contributed to pregnancy with the partner during followup.
Conclusions: Low dose human chorionic gonadotropin appears to maintain semen parameters in hypogonadal men on testosterone replacement therapy. Concurrent testosterone replacement and human chorionic gonadotropin use may preserve fertility in hypogonadal males who desire fertility preservation while on testosterone replacement therapy.
**************************************************
Low-dose human chorionic gonadotropin maintains intratesticular testosterone in normal men with testosterone-induced gonadotropin suppression. Randomized controlled trial
Coviello AD, et al. J Clin Endocrinol Metab. 2005.
Abstract
In previous studies of testicular biopsy tissue from healthy men, intratesticular testosterone (ITT) has been shown to be much higher than serum testosterone (T), suggesting that high ITT is needed relative to serum T for normal spermatogenesis in men. However, the quantitative relationship between ITT and spermatogenesis is not known. To begin to address this issue experimentally, we determined the dose-response relationship between human chorionic gonadotropin (hCG) and ITT to ascertain the minimum dose needed to maintain ITT in the normal range. Twenty-nine men with normal reproductive physiology were randomized to receive 200 mg T enanthate weekly in combination with either saline placebo or 125, 250, or 500 IU hCG every other day for 3 wk. ITT was assessed in testicular fluid obtained by percutaneous fine needle aspiration at baseline and at the end of treatment. Baseline serum T (14.1 nmol/liter) was 1.2% of ITT (1174 nmol/liter). LH and FSH were profoundly suppressed to 5% and 3% of baseline, respectively, and ITT was suppressed by 94% (1234 to 72 nmol/liter) in the T enanthate/placebo group. ITT increased linearly with increasing hCG dose (P < 0.001). Posttreatment ITT was 25% less than baseline in the 125 IU hCG group, 7% less than baseline in the 250 IU hCG group, and 26% greater than baseline in the 500 IU hCG group. These results demonstrate that relatively low dose hCG maintains ITT within the normal range in healthy men with gonadotropin suppression. Extensions of this study will allow determination of the ITT concentration threshold required to maintain spermatogenesis in man.
To find out if sperm count is normalized in men using hCG plus TRT, several studies have found that 17OH-P blood level is correlated to intratesticular testosterone (ITT) required for the testicles to make sperm, so testing for this hormone could not only save time while optimizing HCG dose/frequency but also eliminate the need to perform testicular aspirations, a very difficult procedure to do. Sperm count does not stabilize until 6-8 weeks after starting hCG plus TRT, so knowing your 17 OH-progesterone blood level can give you a quick way to determine if your hCG dose and frequency is adequate before your first follow-up semen analysis after 8 weeks.
MORE INFORMATION:HCG USE IN MEN





